Utah legislators push controversial bill allowing patients to bring their own blood
2025-02-21 02:16- A bill in Utah mandates healthcare facilities to permit patients to use their own blood or choose their donors for procedures.
- The bill, receiving unanimous support, is driven by concerns over personal choice amidst vaccination hesitance.
- Opponents argue the legislation could compromise blood safety and healthcare delivery.
Express your sentiment!
Insights
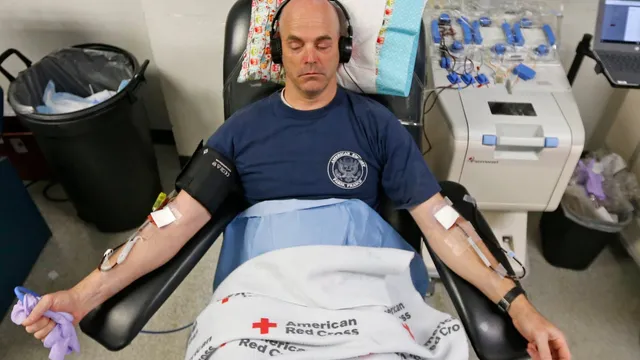
In Utah, legislation is underway that mandates healthcare facilities to allow patients to supply their own blood for medical procedures or to choose their donors. This bill, passed unanimously by the state House, is spearheaded by Rep. Kristen Chevrier, an advocate for patient autonomy, particularly concerning vaccine concerns that have arisen during the COVID-19 pandemic. Although such directed donations are permissible under federal law, they must pass through a comprehensive screening process that some argue limits personal choice. Opponents, including the American Red Cross, are voicing serious concerns regarding the implications of the proposed measure. Their stance emphasizes that allowing patients to select their blood donors could jeopardize the safety of blood transfusions. They argue that more requests for directed donations could divert valuable resources away from individuals in need of lifesaving blood, thereby affecting the overall healthcare delivery system. Medical professionals warn that these requests, driven by personal preference rather than medical necessity, might not represent the safest options for patients in need. Health officials also point out that family or friends may feel undue pressure to donate, potentially withholding crucial health information, which increases the risk of transmitting infectious diseases through directed donations. Despite these clear warnings from health experts, many individuals articulate their desire for the choice of blood sources, underscoring the deeply personal nature of health care. They push back against the prospect of stricter regulations surrounding blood donations while societal apprehensions surrounding vaccines continue to shape healthcare discussions. The political backdrop surrounding the bill reflects a growing divide in public health perspectives, particularly influenced by debates over vaccination. With the legislation headed to the state Senate, the outcome remains uncertain. Still, it exemplifies the tension between individual patient choices and collective health standards, raising vital questions about the safety and efficacy of directed blood donation practices in contemporary medical settings.
Contexts
The impact of directed blood donations is a multifaceted topic that has substantial implications for blood transfusion practices and patient outcomes. Directed donations, which are blood donations made by individuals who specifically choose a recipient—usually a relative or friend—can potentially enhance the psychological comfort of both donors and recipients. The concept is predicated on the belief that receiving blood from a known source may lead to a lower risk of transfusion-transmitted infections and improved compatibility due to shared genetic traits. Furthermore, it may foster a sense of community and responsibility among donors, encouraging a culture of giving that can benefit the healthcare system as a whole. However, while these benefits appear promising, empirical evidence on the clinical outcomes of directed vs. voluntary donations is mixed and warrants further examination. Inclusion of data from various studies shows that voluntary donations generally result in higher-quality blood products, as they tend to attract a larger pool of healthy donors who provide blood regularly and are motivated by altruism rather than personal connections. The American Association of Blood Banks has highlighted that directed donations can sometimes lead to a false sense of security, as family members or friends may have similar risk factors for diseases that can compromise blood safety, undermining the initial motivations behind such donations. Consequently, while the emotional benefits of directed donations cannot be dismissed, health professionals must carefully assess the potential risks associated with reliance on directed donations alone. Moreover, directed blood donations can have significant implications for blood inventory management. Blood banks face challenges in ensuring adequate supplies for recipients in need, and directed donations can sometimes complicate these logistics. If a significant amount of collected blood is specifically earmarked for directed donations, it may result in shortages of universally usable blood products. This could lead to overall diminished availability for emergency situations where timely transfusions are critical. Blood centers must balance the desire to accommodate directed donations with proactive engagement in broader outreach initiatives aimed at boosting donations from the general population. Education and awareness campaigns encouraging voluntary donations can create a more abundant and diverse blood supply, ultimately benefitting a wider range of patients. Moreover, an intentional focus on voluntary donations aligns more closely with the principles of altruism and equity in healthcare. Despite the challenges, promoting a culture of directed blood donations can contribute positively to donor engagement and retention. Personal stories and connections can motivate individuals to take the step to donate, consequently generating more awareness about the ongoing need for blood. Blood donation drives that incorporate directed donations can serve as a platform for broader public education about the importance of blood donation, increasing the overall donor base. Innovative strategies that highlight the impact of the donation and foster personal connections between donors and recipients may enhance the willingness to donate blood, regardless of the type of donation. Community outreach, testimonials, and structured initiatives to bridge the gap between directed and voluntary donations can potentially lead to a more stable blood supply. Ultimately, the overall impact of directed blood donations hinges on a nuanced understanding of their clinical relevance, logistical implications, and potential biases. While they may provide emotional reassurance for certain patients, they must not overshadow the critical importance of fostering a robust environment for voluntary donations. As healthcare systems continue to evolve, ongoing assessments and refinements of blood donation practices will be vital. Acknowledging the need for balanced approaches that incorporate both directed and voluntary blood donation can optimize blood supply and enhance patient safety and outcomes, ensuring that patients receive the best care possible.