FDA expands Ozempic's use to combat chronic kidney disease in diabetes patients
2025-01-30 00:30- The FDA approved Ozempic for treating chronic kidney disease in Type 2 diabetes patients, allowing it to mitigate the risk of worsening kidney function.
- This decision may change how healthcare providers treat chronic kidney disease, which often coexists with diabetes.
- Ozempic's approval signifies broader health benefits of GLP-1 medications in addressing metabolic-related health issues.
Express your sentiment!
Insights
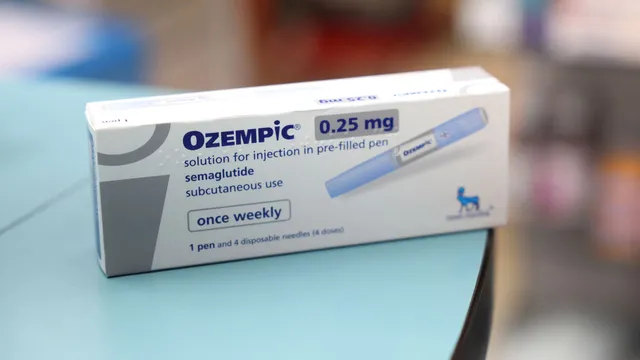
In the United States, the Food and Drug Administration granted approval for Novo Nordisk's Ozempic to be used in treating chronic kidney disease in patients suffering from Type 2 diabetes. This decision was announced on January 28, 2025, and it is expected to significantly impact how healthcare providers approach treatment for patients dealing with kidney issues alongside diabetes. The approval stems from a 2019 study involving 3,500 patients, demonstrating that Ozempic could reduce major kidney and cardiovascular events by 24%. This includes a slower decline in kidney function and a reduction in the risk of heart attack and death. Chronic kidney disease is a leading health issue, affecting approximately 37 million American adults, many of whom also suffer from diabetes. Diabetes increases the risk of kidney complications, with around 40% of Type 2 diabetes patients developing kidney disease. The FDA's endorsement of Ozempic indicates that it can help mitigate the progression of kidney disease and the associated risks of cardiovascular problems. The approval not only affirms the drug's primary function in managing blood sugar levels but also highlights the expanding role of GLP-1 medications in addressing broader health concerns. This landmark approval has significant implications for the healthcare sector, particularly for obesity and diabetes treatment markets. The decision follows intense scrutiny and evaluation of Ozempic in comparison to placebo groups in clinical settings, where it showed a notable reduction in severe kidney complications. Experts have pointed out that many patients often experience overlapping conditions related to diabetes, obesity, chronic kidney disease, and cardiovascular disease, further emphasizing the drug's pivotal role in their treatment plans. As Novo Nordisk navigates a competitive landscape with increasing pressure from other pharmaceutical companies, including Eli Lilly, gaining expanded approval for Ozempic represents a strategic advantage. This approval could change treatment paradigms and improve health outcomes for millions of affected individuals, consequently influencing how professionals view the interconnectedness of diabetes and kidney health in the wider context of public health.
Contexts
The FDA approval process for Ozempic, a glucagon-like peptide-1 (GLP-1) receptor agonist, is a crucial pathway that evaluates the safety and efficacy of this medication for the management of Type 2 diabetes. Ozempic, developed by Novo Nordisk, was submitted for FDA approval following a series of clinical trials demonstrating its effectiveness in lowering blood sugar levels and aiding in weight loss among patients with Type 2 diabetes. The pivotal trial, SUSTAIN-1, along with subsequent SUSTAIN trials, provided robust data regarding its ability to reduce HbA1c levels and achieve significant weight reduction compared to traditional treatments. The FDA's review process is meticulous, involving a thorough analysis of clinical trial results, manufacturing practices, and labeling to ensure that the medication meets the high standards required for public use. As part of the approval process, the FDA evaluates the risk-benefit profile of Ozempic. The submitted data must address various potential adverse effects, such as gastrointestinal issues, thyroid tumors, and pancreatitis, which have been highlighted in the clinical trials. The agency also considers post-marketing surveillance plans necessary for monitoring long-term safety. This structure ensures that if unexpected risks arise after approval, they can be promptly addressed. The outcome of this scrutiny was that Ozempic received FDA approval in December 2017, marking an important addition to diabetes treatment options available to healthcare providers and patients. Once approved, the drug was launched with specific indications, dosing guidelines, and an emphasis on lifestyle modification, which is vital for managing Type 2 diabetes effectively. The prescribing information provides extensive detail on the administration of Ozempic, including subcutaneous injection instructions, dosing increments, and safety information to prevent hypoglycemia. Importantly, education surrounding the medication is essential not only for physicians but also for patients to establish realistic expectations and adherence to therapy. The ongoing communication between healthcare providers and patients plays a pivotal role in monitoring efficacy and any side effects experienced by users. The approval of Ozempic is part of a broader trend within the pharmaceutical industry aimed at developing medications that offer dual benefits of glycemic control alongside weight loss, addressing two critical aspects of Type 2 diabetes management. The FDA's rigorous process exemplifies the agency's commitment to safeguarding public health while facilitating access to innovative therapies. Through continuous post-marketing studies and studies on diverse populations, the safety and effectiveness of Ozempic can be further validated, ensuring it serves as a beneficial component in the management of Type 2 diabetes.